A new report says the seven RAAC hospitals face ‘significant costs and operational risks' as they are not expected to open until 2032-33.
Gareth Davies, head of the NAO, said: ‘The reset of the New Hospital Programme gives the department a firmer platform to deliver long‑term improvements and its ambition to transform hospital infrastructure has real potential provided designs are rigorously tested and programme delivery is well managed.'
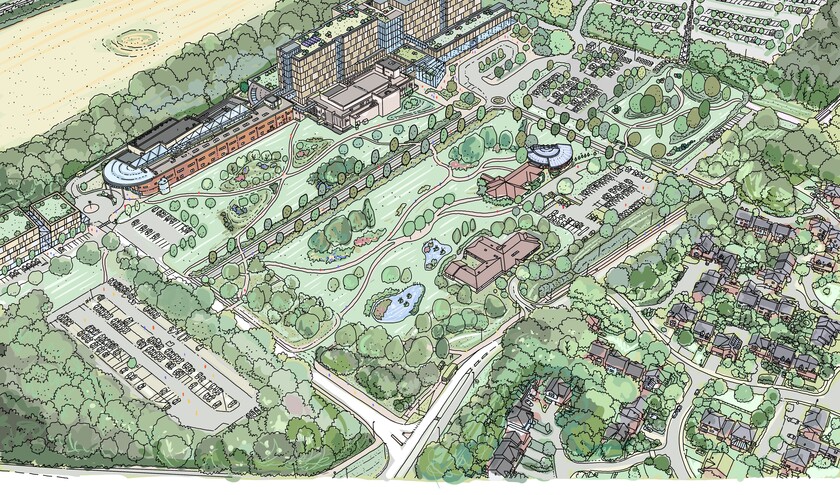
The reset covers 41 hospital schemes, which range from whole new buildings to major refurbishments, and will be carried out in four waves over the next 20 years. An additional five schemes were already complete and open when the programme was reset in January 2025. The final hospitals are expected to be completed in 2045-46.
The NAO warned trusts whose new hospitals or refurbishments will open later will face additional costs to maintain ageing buildings for longer of between £100m and £140m a year.
Around £2bn a year has been allocated to the programme from 2025–26 to 2029–30, rising to £3 bin a year from 2030–31 with a total capital funding of £56bn required, £33bn above the 2023 proposal.
In the 28 Hospital 2.0 schemes, DHSC assumes the number of overnight beds will rise by an average of 6%. The new approach assumes a 92% bed occupancy rather than a ‘riskier' 95% which allows less spare capacity for surges in demand. However, the NAO notes the model requires a major shift of care to the community.
DHSC estimates a £3.10 return for every £1 spent under a centralised programme, compared to £2.70 if individuals trusts built their own hospitals – delivering up to £7.5bn more in measurable benefits, including better emergency and ambulance performance, digital technology benefits and reduced hospital infections due to patients having their own room. If successful, DHSC expects to secure operational benefits from the 2030s, when the first Hospital 2.0 schemes open.
Reaction
Rory Deighton, acute and community care director at the NHS Confederation, said ‘the scale of the capital challenges facing the NHS means that the NHP could never be a panacea, and further private investment in capital is one of the only viable options available to boost capital funding into the NHS'.
Deighton added: ‘We have welcomed the Government giving the green light for private capital to be used to fund the new wave of neighbourhood health centres, but if we are to fix the health service's capital woes this should be extended more widely – particularly to hospitals and mental health services.'
Tim Mitchell, president of RCS England, said: ‘A steadier plan is better than drifting, but patients cannot wait a decade for capacity that we need now. NHS trusts will be pouring scarce funds into patching up old buildings for longer, when that money should be used to create extra operating theatres, securing ring‑fenced beds and making sure that there is enough staff to run them.
‘Our latest surgical workforce census shows surgeons repeatedly blocked by a shortage of theatre space. Unless we fix capacity with further capital investment, the waiting‑times target will stay out of reach.'
Daniel Elkeles, chief executive, NHS Providers, said: ‘Ageing hospital buildings may have to stay in use way past their "use-by" dates, putting patients and staff at risk and costing NHS trusts and taxpayers millions of pounds because some NHP schemes are now not expected to begin construction until 2039.'
A Department of Health and Social Care spokesperson said: ‘This report demonstrates this Government has put the New Hospital Programme on a stable long-term footing after inheriting a plan that was unfunded and undeliverable.
‘We've confirmed a sustainable funding plan and an achievable timetable to deliver all schemes in the programme. We are now getting on with building these much-needed facilities as quickly as possible.
‘We are backing the NHS with £1.6bn across the next four years to safely remove and mitigate RAAC to protect patient and staff safety and deliver a health service fit for the future.'